Valmar Won’t Be the Last: The Hidden Cost of the Cost Model
February 4, 2025
The hidden cost of the cost model is a conversation we can’t ignore.
By now, most of you have heard about the Valmar case. This
heartbreaking situation had devastating consequences, and our deepest
condolences go out to those directly impacted. While no two cases are
identical, the broader issues that contributed to this tragedy were sadly,
foreseeable.
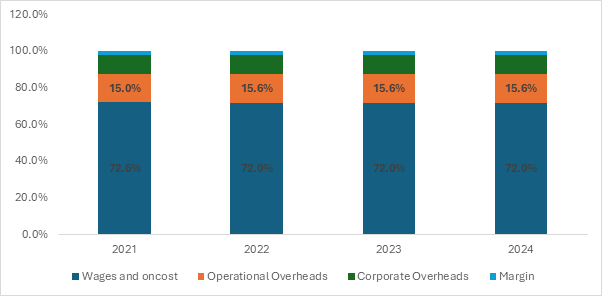
Last week, we saw how the top 10 attendant care providers are experiencing persistent operating losses. This article digs deeper into the SIL cost model to show how real-world factors—such as vacancies and surplus hours—lie mostly outside its formal funding scope. Once corporate overhead is brought down to an ultra-lean level, the remaining levers typically force cuts to direct supports, especially supervision and training. Over time, these reductions weaken the very safety controls essential to good practice and participant outcomes.
The Cost Model’s Efficiency Assumption
A commonly repeated tenet of SIL pricing is:
“The cost model pays a supervisor at SCHADS 3.2, assuming
a 15 FTE span of control.”
To understand how razor-thin these margins can be, let’s
consider a strict 1:3 SIL setting (with no additional
supports):
- 3.54
FTE are required to staff a single 1:3 property fully.
- Under
the cost model’s logic, one supervisor at SCHADS 3.2
overseeing 15 FTEs would manage about 4.24 houses and 12.72
participants.
- In
practice, that means roughly 30+ staff to roster
(counting leave cover), plus an annual turnover that might require six
new hires per year per cluster of houses.
Each 1:3 house often involves higher levels of
complexity—seizure management, mealtime protocols, community participation, or
nuanced social interactions. Even in the best circumstances, a supervisor’s
time is stretched thin.
Now, scale that ratio up to 1:6 or
higher:
- The
same single supervisor could be responsible for double (or
more) the participant load, meaning substantially more support plans,
staff coordination, and incident follow-ups.
- The
cost model doesn’t increase the supervisor’s resourcing to reflect the
increased administrative or clinical oversight needed. It is fixed at the
staffing unit.
- More
participants multiply the demands on that same finite supervisory
bandwidth.
In both scenarios, once you add typical real-world
disruptions—staff sickness, participant transitions, or unexpected
vacancies—supervisors end up pulled away from their primary role of practice
leadership.
Note: While it hasn’t been stated since 2021: we can assume
these assumptions are conserved once we pull categories forward.
But that is just one component of a broader approach built
on peak efficiency. The model:
- Benchmarks
Corporate Overhead
- At
the 25th percentile of providers—meaning providers are expected to run
extremely lean.
- Assumes
robust systems and minimal administrative burden.
- Expects
Stable, Fully Utilised Staffing
- Anticipates
low turnover, minimal absenteeism, and high occupancy (i.e., few
vacancies).
- Supposes
that “surplus hours” (unfunded extra staff time) rarely occur.
While logical on paper, these assumptions quickly
unravel when real-world complexities—such as overhead inefficiencies,
unplanned participant absences, or staff turnover—enter the picture.
Overhead Inefficiencies and Their Impact on Supervision
Under ideal conditions, corporate overhead is minimal yet
sufficient: the provider has efficient HR, technology, and administrative
workflows. In reality, systems immaturity and weak
balance sheets often spill over to supervisors.
- Underfunded
HR leads to slow recruitment processes, pushing line managers and
supervisors into repetitive hiring or onboarding tasks.
- Manual
compliance and record-keeping (due to lack of a proper CRM)
forces supervisors to track participant documents themselves.
- Gaps
in finance or quality systems mean supervisors also become de
facto troubleshooters—spending hours on tasks outside their scope.
Once you reach the hard floor of these overheads—where
there’s simply no more fat to trim—any additional budget shortfall essentially
comes at the cost of frontline support, particularly supervision and training.
Sensitivity Analysis: Validating the Vacancy and Surplus Problem
Our team conducted a sensitivity analysis,
simulating thousands of SIL providers under varying conditions. Two consistent
factors emerged that undermine cost-model sustainability:
Hard line
Once vacancies and surplus exceed 12%, the provider
loses enough operating margin that either overhead must be cut further (already
at a minimum) or direct support must be curtailed.
The analysis showed that once corporate overhead is
lean, vacancy and surplus-hour stress almost inevitably pushes providers
to chip away at supervision and training. This is not a moral
failing, but a structural reality of the current pricing approach.
Why Supervision Suffers First
- Supervisors
Plug Roster Gaps
- When
staff call in sick or there’s an unexpected vacancy, supervisors fill
shifts to maintain participant safety.
- Time
previously earmarked for staff coaching or practice development vanishes,
replaced by frontline coverage.
- Training
Becomes a “Luxury”
- With
margins stretched, formal training budgets are among the first to be
reined in.
- Over
time, staff skills stagnate or degrade, increasing the likelihood of
incidents or suboptimal supports.
- Practice
Leadership Devolves
- Supervisors
spend their days in reactive mode—juggling rosters, incident management,
and admin tasks.
- In-situ
coaching—evidenced by the works of Beadle-Brown, Bigby, and
Mansell—diminishes, robbing staff of real-time feedback crucial for
high-quality support.
Practice Leadership: Introducing the Stakes
Practice Leadership is widely regarded as the
most critical element in delivering safe and effective SIL supports. It
revolves around direct, context-specific oversight:
- Engaged
Observation: Supervisors watch staff in action, providing
immediate pointers or course-corrections.
- Responsive
Coaching: Teams are guided through complex participant
interactions—think de-escalation techniques, behavioural supports, or
medical protocols.
- Proactive
Safety Measures: Supervisors identify early warning signs and
embed preventative strategies rather than reacting after incidents occur.
This leadership style is high effort, high reward—it
reliably improves participant outcomes but is also fragile when
supervisory capacity is squeezed. Once finances force supervisors into
frontline coverage, compliance chores, or constant recruitment, the
high-touch nature of practice leadership is one of the first casualties.
Everything Affects Safety
When even small inefficiencies arise—vacancies, surplus
hours, overhead gaps—they radiate through the entire SIL operation:
- Overhead
shortfalls push admin tasks onto supervisors, reducing time for
coaching.
- Vacancies reduce
incoming revenue, prompting budget cuts to supervision or training.
- Surplus
staffing needs (often for genuine participant safety) go
unfunded, heightening financial strain.
- High
staff turnover (exacerbated by limited training) creates a cycle
of never-ending onboarding, further distracting supervisors.
Each step erodes the ability to maintain consistent,
high-quality support. Indeed, every facet of a SIL
provider—from HR to IT—either conserves or undercuts participant
safety.
Conclusion: Preserving Practice Leadership in the Cost Model
Valmar is unlikely to be the last provider marred by crisis
under the current arrangements. By design, the NDIS pricing model pressures
providers to operate with minimal overhead, leaving no buffer for unexpected
vacancies or essential surplus hours. Once that buffer is gone, the inevitable
cuts fall upon supervision and training—the
two linchpins of safe, person-centred care.
To prevent these near-misses and collapses:
- Acknowledge
Real-World Variances
- Funding
models should accommodate typical fluctuations in occupancy and staff
hours, rather than assuming everything aligns perfectly.
- Provide
for Essential Surplus Hours
- When
participants genuinely need additional support, providers shouldn’t have
to absorb it without any financial offset.
- Protect
Practice Leadership
- Directly
invest in supervisory capacity and training to ensure the high-touch
oversight that underpins safety and quality.
Until these systemic gaps are addressed, SIL providers will
remain perched on a financial knife-edge—forced to cut back on the very
mechanisms (supervision and practice leadership) that guard participants from
harm. Consequently, the risk of recurring incidents akin to Valmar remains
alarmingly high.
At Empathia Group, we understand the critical role of
supervision, training, and sustainable funding in delivering safe, high-quality
support. If your organisation is navigating these challenges, we’re here to
help—offering practical guidance to strengthen systems without compromising
care.
Share this article:
Continue reading Empathia Insights
The Top 10 NDIS Providers in 2024: Difficulty at scale and lessons for the sector
There’s a persistent rumour in the disability sector that the National Disability Insurance Agency (NDIA) is slowly corralling services into...


